Vaginal Prolapse
Home / Vaginal Prolapse
Home / Vaginal Prolapse
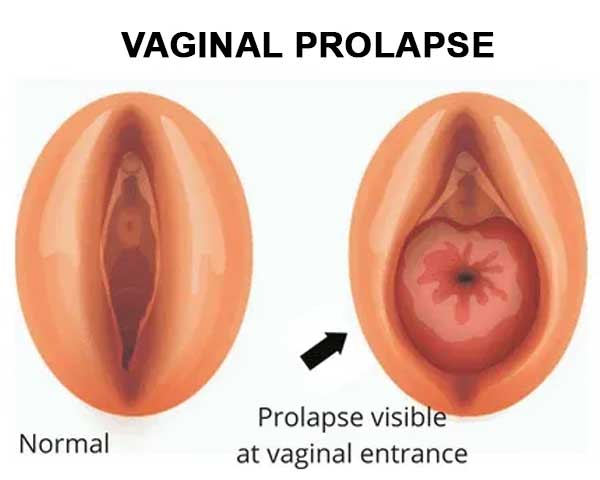
Vaginal prolapse, also known as pelvic organ prolapse, occurs when the structures supporting the pelvic organs, such as the bladder, uterus, or rectum, weaken or stretch, leading to a descent of one or more of these organs into the vaginal canal. This condition can affect women of all ages, but it is more common in older women, particularly those who have given birth multiple times or experienced menopause.
Cystocele (Anterior Prolapse): This involves the descent of the bladder into the vaginal canal. It is often associated with stress incontinence and a bulging sensation in the front wall of the vagina.
Rectocele (Posterior Prolapse): In this type, the rectum bulges into the back wall of the vagina. Women with rectocele may experience difficulty with bowel movements and a feeling of rectal fullness.
Uterine Prolapse: Uterine prolapse occurs when the uterus descends into the vaginal canal. This can happen after childbirth, especially in women who have had multiple pregnancies, and may lead to a feeling of pelvic pressure.
Enterocele: This involves the small intestine pushing into the upper portion of the vagina, creating a pouch-like bulge. Enterocele is less common but can cause discomfort and difficulty with bowel movements.
Childbirth: The strain of vaginal childbirth, especially multiple deliveries, can weaken the pelvic floor muscles and contribute to prolapse.
Aging: The natural aging process can lead to a reduction in collagen and elasticity of the pelvic tissues, making them more prone to prolapse.
Menopause: The decline in estrogen levels during menopause can contribute to a loss of pelvic muscle tone.
Chronic Straining: Conditions that involve chronic straining, such as chronic constipation or heavy lifting, can increase the risk.
Genetics: Some women may have a genetic predisposition to weaker connective tissues, making them more susceptible to prolapse.
Conservative Measures:
Pessaries:
Hormone Replacement Therapy (HRT):
Surgery:
Women experiencing symptoms of vaginal prolapse should consult with a healthcare provider for a proper diagnosis and personalized treatment plan. The choice of treatment will depend on the severity of the prolapse, the specific organs involved, and the impact on a woman's quality of life.